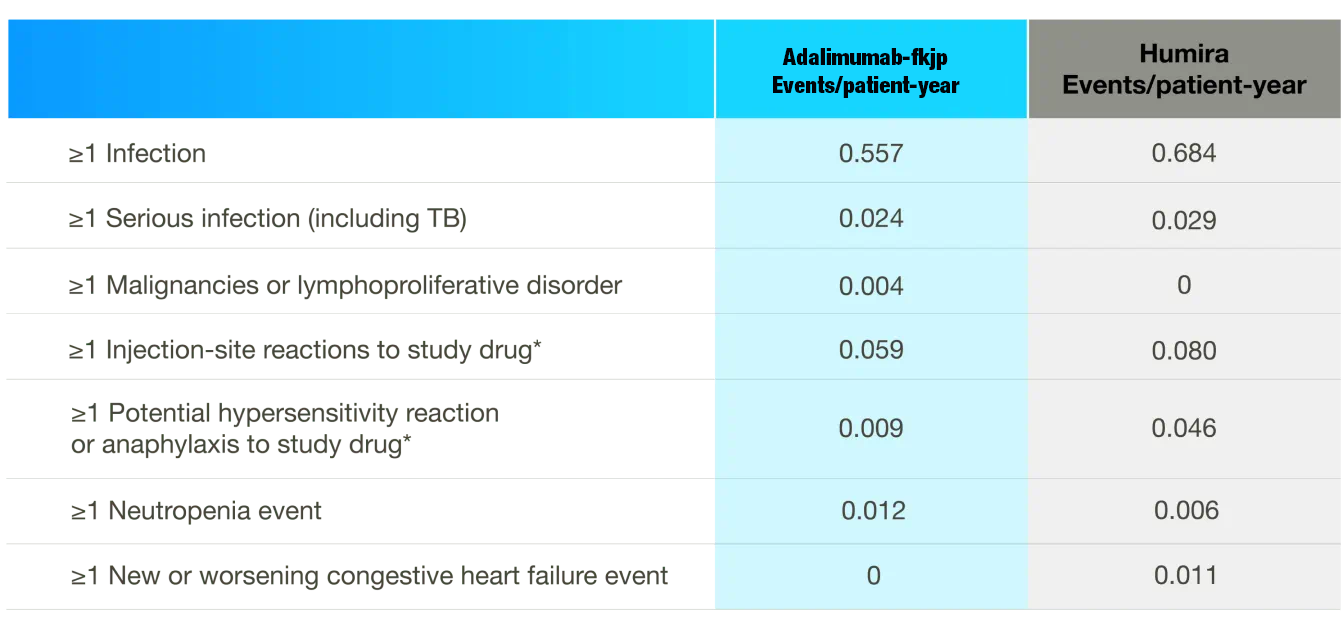
Patients treated with adalimumab products (including Adalimumab-fkjp) are at increased risk for developing serious infections that may lead to hospitalization or death. Most patients who developed these infections were taking concomitant immunosuppressants
such as methotrexate or corticosteroids.
Discontinue Adalimumab-fkjp if a patient develops a serious infection or sepsis.
Reported infections include:
- Active tuberculosis (TB), including reactivation of latent TB. Patients with TB have frequently presented with disseminated or extrapulmonary disease. Test patients for latent TB before Adalimumab-fkjp use and during therapy. Initiate treatment for latent TB prior to Adalimumab-fkjp use.
- Invasive fungal infections, including histoplasmosis, coccidioidomycosis, candidiasis, aspergillosis, blastomycosis, and pneumocystosis. Patients with histoplasmosis or other invasive fungal infections may present with disseminated, rather than localized, disease. Antigen and antibody testing for histoplasmosis may be negative in some patients with active infection. Consider empiric anti-fungal therapy in patients at risk for invasive fungal infections who develop severe systemic illness.
- Bacterial, viral, and other infections due to opportunistic pathogens, including Legionella
and Listeria.
Carefully consider the risks and benefits of treatment with Adalimumab-fkjp prior to initiating
therapy in patients:
1) with chronic or recurrent infection, 2) who have been exposed to TB, 3) with a history of opportunistic
infection, 4) who resided in or traveled in regions where mycoses are endemic, 5) with underlying conditions that may predispose them to infection. Monitor patients closely
for the development of signs and symptoms of infection during and after treatment with Adalimumab-fkjp, including the possible development of TB in patients who tested negative for latent TB infection prior to initiating therapy.
- Do not start Adalimumab-fkjp during an active infection, including localized infections
- Patients older than 65 years, patients with comorbid conditions, and/or patients taking concomitant
immunosuppressants may be at greater risk of infection.
- If an infection develops, monitor carefully and initiate appropriate therapy.
- Drug interactions with biologic products: A higher rate of serious infections has been observed in
RA patients treated with rituximab who received subsequent treatment with a TNF blocker. An
increased risk of serious infections has been seen with the combination of TNF blockers with
anakinra or abatacept, with no demonstrated added benefit in patients with RA. Concomitant
administration of Adalimumab-fkjp with other biologic DMARDs (e.g., anakinra or abatacept) or
other TNF blockers is not recommended based on the possible increased risk for infections and
other potential pharmacological interactions.
Malignancy
Lymphoma and other malignancies, some fatal, have been reported in children and adolescent
patients treated with TNF blockers including adalimumab products. Postmarketing cases of
hepatosplenic T-cell lymphoma (HSTCL), a rare type of T-cell lymphoma, have been reported in patients treated with TNF blockers including adalimumab products. These cases have had a
very aggressive disease course and have been fatal. The majority of reported TNF blocker
cases have occurred in patients with Crohn’s disease or ulcerative colitis and the majority
were in adolescent and young adult males. Almost all these patients had received treatment
with azathioprine or 6-mercaptopurine (6-MP) concomitantly with a TNF blocker at or prior to
diagnosis. It is uncertain whether the occurrence of HSTCL is related to use of a TNF blocker
or a TNF blocker in combination with these other immunosuppressants.
- Consider the risks and benefits of Adalimumab-fkjp treatment prior to initiating or continuing therapy
in a patient with known malignancy.
- In clinical trials of some TNF blockers, including adalimumab products, more cases of malignancies
were observed among TNF-blocker-treated patients compared to control patients.
- Non-melanoma skin cancer (NMSC) was reported during clinical trials for adalimumab-treated
patients. Examine all patients, particularly those with a history of prolonged immunosuppressant or
PUVA therapy, for the presence of NMSC prior to and during treatment with Adalimumab-fkjp.
- In adalimumab clinical trials, there was an approximate 3-fold higher rate of lymphoma than
expected in the general US population. Patients with chronic inflammatory diseases, particularly
those with highly active disease and/or chronic exposure to immunosuppressant therapies, may be
at higher risk of lymphoma than the general population, even in the absence of TNF blockers.
- Postmarketing cases of acute and chronic leukemia were reported with TNF blocker use.
Approximately half of the postmarketing cases of malignancies in children, adolescents, and young
adults receiving TNF blockers were lymphomas; other cases included rare malignancies
associated with immunosuppression and malignancies not usually observed in children and
adolescents.
Hypersensitivity
- Anaphylaxis and angioneurotic edema have been reported following administration of adalimumab
products. If a serious allergic reaction occurs, stop Adalimumab-fkjp and institute appropriate
therapy.
Hepatitis b virus reactivation
- Use of TNF blockers, including HULIO, may increase the risk of reactivation of hepatitis B virus (HBV) in
patients who are chronic carriers. Some cases have been fatal.
- Evaluate patients at risk for HBV infection for prior evidence of HBV infection before initiating TNF
blocker therapy.
- Exercise caution in patients who are carriers of HBV and monitor them during and after Adalimumab-fkjp treatment.
- Discontinue Adalimumab-fkjp and begin antiviral therapy in patients who develop HBV reactivation.
Exercise caution when resuming Adalimumab-fkjp after HBV treatment.
Neurologic reactions
- TNF blockers, including adalimumab products, have been associated with rare cases of new onset
or exacerbation of central nervous system and peripheral demyelinating diseases, including
multiple sclerosis, optic neuritis, and Guillain-Barré syndrome.
- Exercise caution when considering Adalimumab-fkjp for patients with these disorders;
discontinuation of Adalimumab-fkjp should be considered if any of these disorders develop.
- There is a known association between intermediate uveitis and central demyelinating disorders.
Hematologic reactions
- Rare reports of pancytopenia, including aplastic anemia, have been reported with TNF blockers. Medically significant cytopenia has been infrequently reported with adalimumab products.
- Consider stopping Adalimumab-fkjp if significant hematologic abnormalities occur.
CONGESTIVE HEART FAILURE
- Worsening and new-onset congestive heart failure (CHF) have been reported with TNF
blockers. Cases of worsening CHF have been observed with adalimumab products; exercise
caution and monitor carefully.
Autoimmunity
- Treatment with adalimumab products may result in the formation of autoantibodies and, rarely,
in development of a lupus-like syndrome. Discontinue treatment if symptoms of a lupus-like
syndrome develop.
Immunizations
- Patients on Adalimumab-fkjp should not receive live vaccines.
- Pediatric patients, if possible, should be brought up to date with all immunizations before initiating
Adalimumab-fkjp therapy.
- Adalimumab is actively transferred across the placenta during the third trimester of pregnancy and
may affect immune response in the in utero exposed infant. The safety of administering live or liveattenuated
vaccines in infants exposed to Adalimumab-fkjp in utero is unknown. Risks and benefits
should be considered prior to vaccinating (live or live-attenuated) exposed infants.
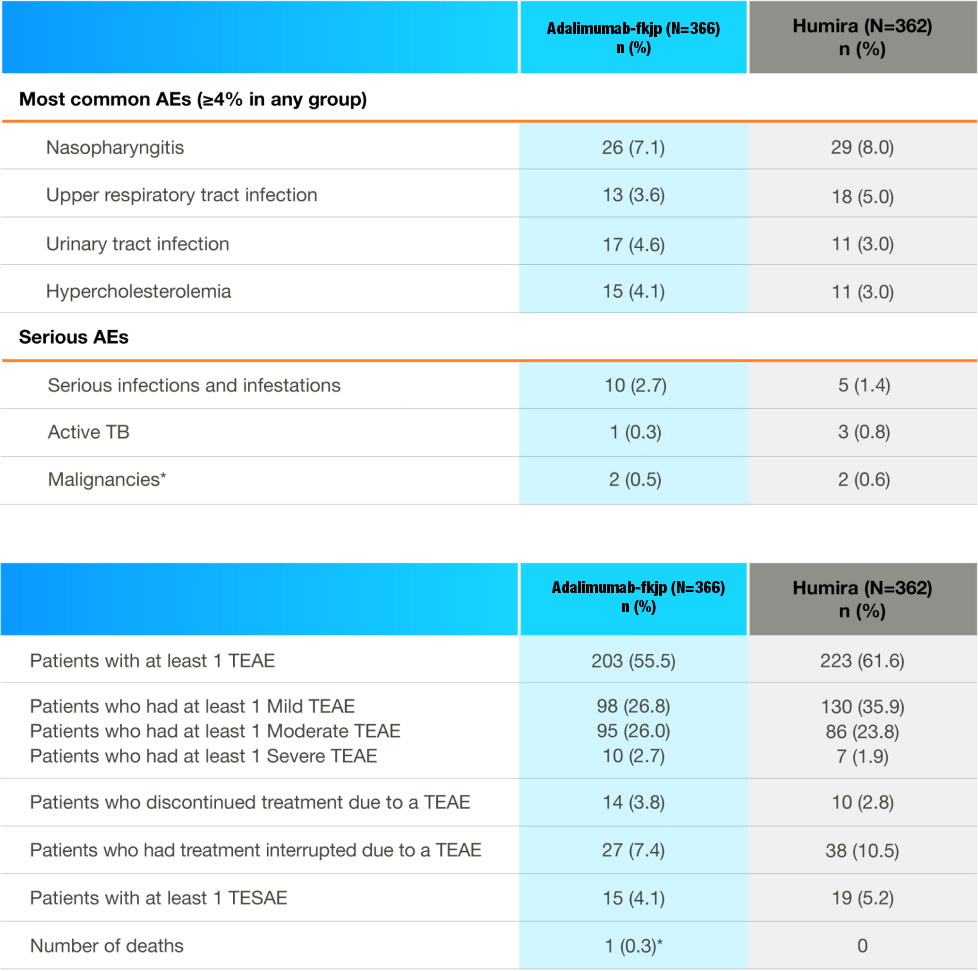
Adverse reactions
- The most common adverse reactions in adalimumab clinical trials (>10%) were: infections (e.g.,
upper respiratory, sinusitis), injection site reactions, headache, and rash.